Supporting the discussion for the lifting of mask mandates using scientific data
“It is difficult to free fools who revere their chains” – Voltaire
Within 24 hours, it would appear that almost all ~330 million people in the United States had a “hot take” on Governor Abbots decision to lift the state of Texas’ mask mandate and allow all businesses, regardless of trade, to open to 100% capacity in a week’s time (Wednesday March 10th). From Joe Biden declaring the move “Neanderthal thinking” and Robert Francis (Beto) O’Rourke claiming in an msnbc interview, “…to be clear, and to be honest with everybody, this action is going to kill more Texans than already died from this pandemic.”, is there any possible defense for this action from the Texas Governor? Without reading the rest of the article I will make the claim that one can come to a conclusion, looking at the masking data and the past year of recommendations from the experts, that choosing not to enforce the Texas mask mandate and broad mask mandates in general is reasonable.
I will begin with three different examples at a very broad level. Two will show the lack of correlation of response or action to outcome regarding SARS-CoV-2 deaths and one will display the mortality by age group of SARS-CoV-2.
To date, multiple states other than Texas have lifted or in some cases never enforced a general mask mandate for the public: Montana, Iowa, North Dakota, Mississippi, Alaska, Arizona, Florida, Idaho, Missouri, Nebraska, Oklahoma, South Carolina, South Dakota, and Tennessee with Texas being the largest state by far to lift the mandate by population. (AARP mask mandate list)
Figure 1: States (death per million) With no mask, March 2021 (Source:Beckershospitalreview.com)
| States | Deaths per million from SARS-CoV-2 |
| Alaska | 49th |
| Arizona | 6th |
| Florida | 26th |
| Georgia | 23rd |
| Idaho | 42nd |
| Iowa | 16th |
| Mississippi | 5th |
| Missouri | 29th |
| Montana | 33rd |
| Nebraska | 38th |
| North Dakota | 11th |
| Oklahoma | 36th |
| South Carolina | 19th |
| South Dakota | 8th |
| Tennessee | 18th |
| Texas | 24th |
Figure 1 shows that at the very least the mask mandates alone have had a non predictive impact on the deaths from SARS-CoV-2. This point has been addressed ad nauseum from several sources dictating that rates may be more clearly correlated to a combination of actions such as social distancing, masking, vaccination, limited interaction, removal of indoor dining and shopping, limited air travel, and a host of other restrictions. The data however are not as clear as the combination of aforementioned actions would suggest; just going by the list of SARS-CoV-2 death rates by state once again we will see the top 10 states for Covid deaths have a combination of States that handled the outbreak differently (Figure 2). Five of the ten states are Democratic and the other half are Republican. Six are in the northern half of the continental US and 4 in the Southern half (3 of which have a coastline along the Caribbean Sea). New Jersey (number 1 on the list) is the most densely populated State. New York has the largest population (4th of all 50 states and US territories). Rhode Island and South Dakota are 44th and 47th respectively regarding population size with Rhode island being the 4th most densely populated state and South Dakota being the 52nd most densely populated of all 50 states and US territories. States like New York enacted nearly complete lock downs at certain points in the pandemic response, while states like South Dakota never declared jobs be shut down or which jobs were even deemed “essential”. This listing can go on for a considerable number of finer and finer details, but the main take away should be that the States handled the outbreaks differently and with this variety came successes and failures showing that a one size fits all response to COVID-19, including the enforcement of mask policies, is not prudential.
Alaska for example is not the same as New York (obviously), but it should follow that a potential response that works in Alaska may not work in New York. A federalist approach in this case with federal support seems to me much more sensible; the states know their own needs better than the federal government and should in fact be in charge of their own response.
Figure 2: States with highest Covid deaths (death per million), March 2021 (Source:Beckershospitalreview.com)
| States | deaths per million from SARS-CoV-2 |
| New Jersey | 1st |
| New York | 2nd |
| Rhode Island | 3rd |
| Massachusetts | 4th |
| Mississippi | 5th |
| Arizona | 6th |
| Connecticut | 7th |
| South Dakota | 8th |
| Louisiana | 9th |
| Alabama | 10th |
Early on in the pandemic, several characteristics of the SARS-CoV-2 virus’ impact on the population could be seen even before the first documented case in the US occurred. One of the most startling, indicative, and consistent characteristics was the seemingly discriminatory aspect of the virus for the elderly population. Looking across the pond at Italy for a brief moment, according to the John Hopkins Covid-19 global tracker (Covid global tracker) by March 3rd, 2020 there were a recorded 79 deaths from SARS-CoV-2, the youngest being 55 suffering from chronic illness, one 61 year old doctor and the other 77 ranging in ages from 63 – 91 with the majority having multiple underlying serious illnesses. By March 10th, 2020, the number of dead from SARS-CoV-2 jumped to 463 (a roughly 600% increase in number of deaths from the previous week) with the average age of death at 81. This trend describing impact by age has followed, statistically speaking, into the United States. This data maintained the same trend from Italy to Spain to Singapore. The website Statista breaks down total COVID-19 deaths as of February 13th in the United States. I am choosing this date as vaccines had just reached the 1 million doses administered per day value, so it is likely that by the end of February and beginning of March vaccinations will begin to strongly skew data (for the better in all likelihood adding protection to the most vulnerable group).
Figure 3: SARS-CoV-2 deaths by age in the US, Statista, February 13th
| Age | Deaths from SARS-CoV-2 (460,234) | Percentage |
| Under 1 | 45 | 0.00978% |
| 1 – 4 | 23 | 0.00500% |
| 5 – 14 | 72 | 0.01564% |
| 15 – 24 | 648 | 0.14080% |
| 25 – 34 | 2922 | 0.63489% |
| 35 – 44 | 7711 | 1.67545% |
| 45 – 54 | 21251 | 4.61743% |
| 55 – 64 | 54134 | 11.7623% |
| 65 – 74 | 99019 | 21.5149% |
| 75 – 84 | 128192 | 27.8537% |
| 85 and older | 146217 | 31.7701% |
The reason for displaying this age segue in figure 3 is to show this is one of the few consistent data surrounding SARS-CoV-2 since the beginning of the outbreak the scientific community has collected. The age breakdown along with certain comorbidities such as obesity are extremely strong predictors of populations that will be severely impacted from the virus. We can use this data to make much more precise and targeted approaches and responses to the developing outbreak instead of these total encompassing and highly restrictive policies. We can send relatively protective masks such as the N – 95 masks to nursing homes, and citizens with comorbidities can request to be in the front of the line to receive shipments of the protective masks, while not straining supply by enticing everyone to mask when it is not clear the prevention writ large that kind of masking has.
These broad, bird’s eye view observations bring me to the practice of masking, and for that matter the double masking and all forms of facial coverings with respect to SARS-CoV-2. It goes without saying that masks have been a contentious issue among Americans since the beginning of the pandemic. The justifications for mass masking had a lot more scientific basis at the beginning of the pandemic when we had little to no understanding of the spread of this disease. At that point in time it was almost seen as a scientifically conservative approach, similar to a, “well it’s not hard to put on a mask and it might help so why not?” attitude. As the data has come out, the data for masking en masse at all times as a population becomes quite a bit more questionable.
*Before moving on I want to preface that protocol driven masking in the proper setting and environment has shown to be effective. For example, a surgeon donning a surgical mask for a surgery is properly applying the mask for its intended use in that masks intended environment. The mask is expected to perform efficiently in this setting.*
The US Surgeon General in a tweet on February 29, 2020 stated:
“ Seriously people – STOP BUYING MASKS!
They are NOT effective in preventing general public from catching #Coronavirus, but if healthcare providers can’t get them to care for sick patients, it puts them and our communities at risk!”
(CNN article covering Surgeon General, “No Mask” tweet)
Fauci had it absolutely correct in an interview for 60 minutes with Dr. John LaPook in March of 2020:
“Now when you see people and look at the films …China… South Korea… whatever it is, where everyone is wearing a mask. Right now in the United States people should not be walking around with masks.” – Fauci
“You’re sure of it, ‘cause people are listening really closely to this.” – LaPook
“Right now people should not be walk—there’s no reason to be walking around with a mask. When you’re in the middle of an outbreak wearing a mask might make people feel a little bit better (with air quotes) and it might even block a droplet but it’s not providing the perfect protection that people think that it is. And often there are unintended consequences, people keep fiddling with the mask and they keep touching their face.” – Fauci
(Fauci 60 Seconds Interview segment)
This was the traditional understanding in epidemic and outbreak literature; masks may be a preventative measure for the outbreak, but in the midst of outbreak they are not nearly as effective. Within a week of the above interview, officials were telling the public to stop buying up masks, that they weren’t necessary only for a few more weeks to pass and public health officials, including Fauci and the surgeon General Jerome Adams, to then inform the public as a whole to wear masks and shelter in place. The reason both suggested to the public to stop buying masks was that in reality the healthcare providers needed them and they did not trust the public with leaving enough masks for the healthcare providers in the hospitals addressing patients with SARs-CoV-2. The science has not been particularly clear on the effectiveness of masks in preventing the spread of SARS-CoV-2 outside of controlled environments. Not only with the examples above, but around the world countries with strict masking and isolation such as England and Germany in Europe, Canada in North America, Brazil in South America, have seen spikes and wanes of virus cases that seem to be independent of the strictness of the mask mandate (Covid global tracker).
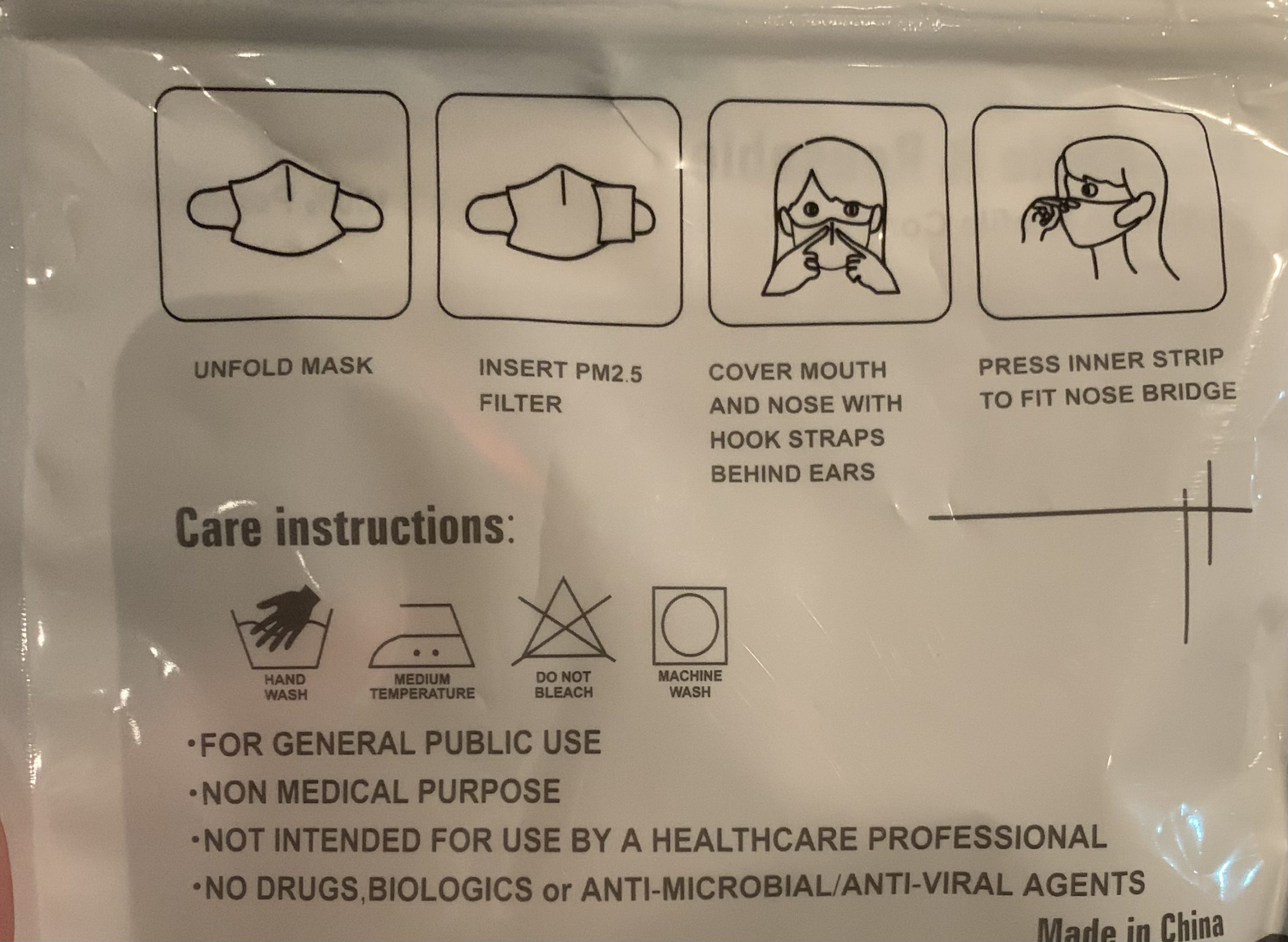
Surgical masks are typically employed in enclosed controlled environments to prevent droplets leaving the mouth during expiration and permeating the immediate vicinity of the breather. A classic example of proper application of a surgical mask is surgeons performing a surgery. The surgical mask offers limited protection to the mask wearer from external particles entering their airway, rather, it is worn to protect others (namely the exposed patient) in the room from droplets. Surgical masks may offer very limited protection to the wearer from particulate or droplet inhalation and several debates have occurred as to protocol in hospital settings for said masks. ( Surgical Mask Discussion 2014)
For a mask to act in a protective manner to the wearer from inhalation risks, it has to form a seal around the nose and mouth. Cloth and surgical masks typically don’t create the kind of seal required for protection. The N95 masks offer a level of protection to the wearer in part due to the filtration system built into the design of the mask, but also in the mask’s ability to form an airtight seal. The seal can also be impacted by facial hair and other features which is why these types of masks typically need to be individually “fitted” before ensuring the maximum level of protection they can offer.
These small details are important and often go neglected in favor of a simplistic message, “wear mask or a face covering”. These and other details are why Dr. Fauci spoke candidly and honestly about the state of masking early on in the pandemic. Once a highly infectious respiratory disease is in a community, unless everyone dons fitted masks correctly, and ensures proper maintenance and care of those masks (a practically impossible task to ask of every member of a population), the masks are not going to be what makes the difference in outcome of spread.
All this being said, for months on end citizens were entering stores wearing surgical masks, cloth masks, bandanas, gaiters, balaclavas, and other assorted face coverings to appease the rules. These rules were being followed despite any scientific data demonstrating efficacy of these face coverings and some studies demonstrating face coverings like gaiters actually increasing the likelihood of spread of SARS-CoV-2 (Droplets Study). A study conducted in 2015, the first randomized control trial (RCT) of this size, analyzed the efficacy of cloth masks relative to medical masks regarding infection rates of clinical respiratory illness and influenza like illness amongst hospital healthcare workers in 14 different hospitals with over 1600 participants. The study demonstrated that the rates of infection among cloth mask users were statistically significantly higher than medical mask users and the researchers concluded with recommending against the use of cloth masks in these settings (RCT of cloth masks in hospital setting).
Without abatement, stories have been regularly released stating airlines having kicked families off for toddlers refusing to keep the mask on (Spirit airlines story) or restaurants having kicked out patrons putting their shirts over their mouths while simultaneously allowing bandana wearing guests to dine with leisure. Again there are no studies I have seen showing airplanes as sources or causes of wide spread break outs for SARS-CoV-2, and likewise I have found no studies showing that bandanas are significantly safer in protecting others from droplets versus shirts worn over the mouth and nose. The droplet study showed all forms of cotton masking, which might behave similar to a cotton shirt over the mouth (speculation), performed significantly better than the bandana at preventing droplets from spreading. These examples highlight some of the mixed messaging and lack of scientific soundness permeating throughout the culture regarding masks.
One of the most glaring hypocritical moments of the pandemic (of which there have been many) was the full support of active protests in large numbers during the lockdowns of a pandemic by over one thousand public health professionals, infectious disease professionals, and community stake holders. This was actually documented in a penned letter in June of 2020 where these officials supported protestors gathering by the tens of thousands to march in close proximity through the streets of major US cities to protest racism. The issue here is these officials, who by self-admission are experts in this field, knew how virulent the disease was at the time and still actively supported such reckless public health behavior. The following is a quote from the letter that to my knowledge has zero scientific evidence supporting the claim that these officials make anyways.
“…We support them [protests] as vital to the national public health and to the threatened health specifically of Black people in the United States. We can show that support by facilitating safest protesting practices without detracting from demonstrators’ ability to gather and demand change. This should not be confused with a permissive stance on all gatherings, particularly protests against stay-home orders. Those actions not only oppose public health interventions, but are also rooted in white nationalism and run contrary to respect for Black lives…”
For reference here is the full letter (Covid Protest Letter)
This example speaks for itself, but one should at least logically find some difficulty with scientific experts recommending all of the correct, public pandemic behavioral practices during this pandemic and then, seemingly arbitrarily, deciding which mass events will be covid spreaders and which won’t. If the other measures and masks particularly were as effective as they claim, any form of protest would be ok so long as proper masking is adhered to. On the flip side, if masks don’t really make a difference then, again, any protest would be ok. It’s the fact that they are deciding which events the masks will work for and which they won’t that should give pause to people following the experts’ recommendations. Again, no scientific evidence has been used to support these claims.
Back to Texas, it has now been well over a month since Texas removed the mask mandate and allowed for business to 100% reopen. This does not mean no masks, rather, my understanding is that any private entity can request patrons wear a mask while on their property but there is no penalty in public spaces if citizens decide to not wear a mask. Covid cases in Texas have overall plummeted and not risen significantly again in the month and a half since the implementation of this policy (Texas Covid Cases). This is, as with a lot of the pandemic responses, multifactorial, but if I were to wager I would posit that this drop in covid case numbers is due in large part to both people who have gotten covid and recovered and the vaccination roll out. The vaccine has proven to be extremely efficacious against the virus, with the Moderna and Pfizer vaccines sporting an efficacy of 94% to SARS-CoV-2 (Vaccine efficacy). Studies have also been released showing a very robust immune response memory to SARS-CoV-2 (Immune Memory Study). At the very least, the predictions of politicians such as Beto O’Rourke have proven to not come true, which is a great thing. Those predictions and dictates should be platforms to increase dialogue on responses and actions including the efficacy of mask usage at the national scale in tempering the virus. It should also be acknowledged when the lifting of the mask mandate did not result in said predictions.
Conclusion:
I am not making the argument that masks don’t work, again in their proper setting and with proper maintenance different masks offer different effective uses. My argument is also not that there is no scientific evidence that masks work, again used for their intended purpose masks can be highly effective and the data show this. My argument in this essay was two fold:
- Simply that the data both through policy effectiveness and scientific study on mask use and effectiveness allow for reasonable debate on whether the mandates on masks should be in place.
- The experts guiding the policy have shown to be arbitrary in their decision making on when masks are effective.
These two arguments do not mean masks are not effective only that it is reasonable to question the efficacy of widespread masking and the debate should be had with both sides preparing their scientific defenses.
The data provided here was only a tiny fraction and with any scientific process and endeavor I encourage everyone who reads this to go out and do some research on topics you find interesting. I implore you to read both sides, give each position the benefit of the doubt that the person making the claim is doing so in good faith, and come to a well-founded and defendable position whatever that may be. Until next time.
-Festina lente-
Gaston Casillas